Spinal osteochondrosis is a degenerative-dystrophic lesion of the intervertebral disc, vertebral body, ligament apparatus, in which bone and cartilage tissue of the cervical, thoracic and lumbar spine is destroyed.
Pathology affects the entire motor segment of the spine, discs, both vertebral bodies, adjacent nerve and muscle structures. The disease is often referred to as the “disease of civilization”, which is associated with upright posture and stress on the spine on a daily basis.
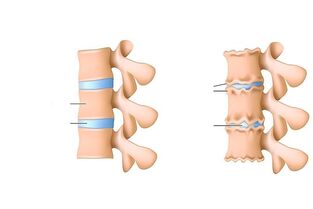
The leading causes of spinal osteochondrosis are microtrauma during physical exercise, unhealthy diet, inactive lifestyle and even genetic predisposition. If the disease progresses, then the intervertebral disc and its adjacent structures suffer first. The middle part of the disc changes, resulting in the loss of shock-absorbing properties on the vertebrae, resulting in cracks and thinning forming on the fibrous ring.
American statisticians say that the first reason for limiting the activity of people under the age of 45 is pain in the spine and cervix. A large number of city dwellers, drivers, who spend most of their time in a sitting position, reloading the spine, are at risk.
Osteochondrosis is the cause of more than 70% of back pain cases. The risk of this disease increases with age.
Etiology and pathogenesis of spinal osteochondrosis
Osteochondrosis of the spine has a long-term pathogenesis (from several months to several decades). It depends on the factors that influence the development of the disease.
Risk Factors:
- Age. Parents (over 60) are at risk. In people under the age of 35, the disease is rare. As a result of age-related changes, disorders occur on the background of human hormones, which makes muscle tissue and blood vessel walls more porous, which means more susceptible. This provokes metabolic disorders, burdening the intervertebral disc.
- Autoimmune diseases that can assume cartilage tissue are foreign and begin to destroy them.
- Spinal injuries. This is one of the main causes of the development of osteochondrosis in young people. It is believed that more than half of people with spinal cord injury at a young age suffer from spinal osteochondrosis in old age.
- Overweight, which reduces the wear of the intervertebral disc. The cartilaginous disc serves as a type of shock absorber for the spine, which ensures its movement during physical activity, walking, running, etc. , And protects bone tissue from the destruction and emergence of microcrats. The severity of the extra weight makes the load stronger, which accelerates the process of destruction of the cartilaginous disc.
- Kaki rata.
- Genetic predisposition.
- Diseases of the endocrine system, which provoke metabolic disorders, which in turn negatively affect the condition of cartilage tissue.
Osteochondrosis can be in a state of "inactivity" for a long time. Many patients find out about this disease in the presence of severe pain, when dystrophic processes in cartilage tissue have damaged nerve roots.
There are such stages in the pathogenesis of spinal osteochondrosis:
- Violation of blood circulation in the intervertebral disc and adjacent structures.
- Hormonal and metabolic disorders in the body and intervertebral discs, in particular.
- Pulp nucleus degradation process. At this stage, the structure of the intervertebral disc changes - the nucleus decreases, the disc itself becomes thinner, the load on the fibrosus annulus increases, which requires various stratification, microcirculation, and sometimes rupture.
- Intervertebral disc protrusion - protrusion of intervertebral disc tissue, often towards the spinal canal, pinches it, causing severe pain.
- Intervertebral hernia. The development of protrusion causes destruction of the ligaments, changes in height and shape of the disc, which in turn provokes the formation of a hernia.
- Radicular artery compression.
- Chronic lack of blood supply to the spinal cord.
Symptoms of osteochondrosis of the spine
As osteochondrosis develops, pathology appears in the intervertebral disc and in the cartilage itself, which then overlaps and can provoke the appearance of an intervertebral hernia.
Symptoms can be general and specific, characteristic of pathological changes in cartilage, intervertebral discs, and adjacent tissues.
The first signs of osteochondrosis should be mentioned back pain, numbness of the vertebrae, limited movement, increased pain during physical exercise.
Specific symptoms of osteochondrosis:
- Cervical osteochondrosis is characterized by impaired blood circulation, which causes dizziness, pain and tinitis, headaches. The brain is less enriched with oxygen and nutrients, as a result of which a person experiences stress.
- Osteochondrosis of the thoracic region, often accompanied by intercostal neuralgia. There is pain in the chest and ribs.
- Osteochondrosis of the lumbar spine provokes the development of lumbago, lumbosacral (sciatica) and lumbar sciatica. With sciatica, the sciatic nerve is affected, pain and hypotension in the back, as well as hypotension in the calf, are observed.
Symptoms of cervical osteochondrosis:
- Cirvicalgia - pain in the cervical spine. The nature of the pain varies (dull, sharp, exacerbated by tilting the head and trunk, when coughing), depending on the factors that affect this part of the spine.
- Cervicobrachialgia - pain in the cervical spine, radiating to the arms, numbness.
- Rthrthrosis of the back shoulder and arthritis - pain in the shoulder joint, in the collarbone, restricts the movement of the arms from top to bottom.
- Epicondylosis - pain in the elbow joint, limited movement.
- Vertebral artery syndrome - so-called cervical migraine, head and cervical headaches, nausea, occasional vomiting, impaired coordination of movements - shock when walking, tinnitus.
One of the most common signs of cervical osteochondrosis is impaired blood circulation, which often causes dizziness, fainting and headaches.
Symptoms of breast osteochondrosis:
- Thoracalgia - chest pain, pain associated with immobility (indicated by prolonged sitting, at night), exacerbated by physical activity, deep breathing, coughing.
- Heart syndrome.
- Posterior chest wall syndrome - pain in the shoulder blade area, pain sensation depends on body position.
- Anterior scalene muscle syndrome.
- Truncalgic syndrome - pain in half of the chest.
- Increased intercostal neuralgia.
Symptoms of lumbar osteochondrosis:
- Lumbodynia - pain in the lower back, lumbago. The patient feels uncomfortable when trying to sit or stand. The pain is exacerbated by physical activity, coughing, breathing deeply, bending over.
- Lumboischialgia - pain in the lower back, radiating to the legs. There may be paresthesia, numbness of the legs, muscle cramps, and joint pain.
- Vascular syndrome - it debuts with compression of blood vessels, is not accompanied by pain, weakness in the muscles observed, cone syndrome - weakness in both legs, dysfunction of the pelvic organs.
Symptoms of osteochondrosis in the lumbar spine are various. This part of the spine is loaded more than the others.
Diagnosis of spinal osteochondrosis
At the first back pain, an examination should be done to determine the cause of the pain. Osteochondrosis is a disease that is difficult to diagnose, as pain can be caused by other pathologies not related to the spine. Patients need consultation from several specialists: neurologists, first of all, orthopedists, vertebrologists.
Methods for the diagnosis of osteochondrosis:
- Radiography. It is performed to accurately determine the height of the intervertebral disc or the change in the structure of the vertebrae, the change in the diameter of the hole between the vertebrae. X-rays are most often performed in two positions - lying on your back and on your side. Two different picture projections allow you to determine the presence of pathology more accurately. Sometimes x-rays are taken with the lower jaw down.
- MRI and CT. MRI results are considered more accurate and help to quickly determine the localization of segments affected by pathology, the presence or absence of intervertebral hernias, and root compression.
- Laboratory tests: blood tests to determine the level of calcium in the blood and the rate of erythrocyte deposition. Laboratory tests were prescribed by the first, recently, based on these results, doctors directed him to hardware diagnostics.
It is important to distinguish spinal osteochondrosis in a number of other diseases with a similar clinical picture, for example: neoplasms of the spine that are oncological, violation of the integrity of cartilage tissue, inflammation, intermittent claudication, cyst formation in internal organs, urolithiasis, gastritis, ulcers, stomach, angina pectoris, nervous system disorders. For this purpose, studies on the digestive system, nervous system, and blood circulation can be determined. The following diagnostic methods are used - cardiogram, ultrasound, electroencephalography, endoscopic examination (digestive organs).
Complications of osteochondrosis
Often, the disease is accompanied by neurological complications:
- Stage. Complications caused by protrusion - painful sharp shooting sensation.
- Stage. Radiculitis, which is characterized by pain syndrome and other symptoms, depends on the localization of radiculitis.
- Stage. Pathology of the roots and spinal cord, the presence of intervertebral hernias. Often, muscle paresis occurs, resulting in paralysis of the entire body.
- Stage. Violation of blood circulation and blood supply to the entire spinal cord. Symptoms: persistent severe back pain, paralysis of certain muscle groups, spinal ischemic stroke.
Treatment of spinal osteochondrosis
The process of treating any type of osteochondrosis pursues one purpose - to relieve pain, to prevent damage and deformation of spinal tissue. Treatment can be done conservatively or surgically. The type and method of treatment is determined individually for each patient, based on the diagnosis (stage, type of disease, general well-being of the patient).
In the acute period of pain syndrome, it is recommended to rest and relax, anti-inflammatory drugs (dicloberl, voltaren), injections of antispasmodic mixtures, vitamin B, preparations for grinding - rileaf dye, larkspur, etc. , can be prescribed when the syndromethe pain is gone. physical education and physiotherapy (diadynamic currents, electrophoresis, magnetotherapy).
Conservative treatment takes about two months. In addition to the treatment methods listed, massage, manual therapy, reflexology, and extraction can also be used. The outcome of conservative treatment directly depends on the patient's perseverance and perseverance.
There is also a surgical treatment method, used when there is an intervertebral hernia over the age of six months, compression of the spinal cord root due to narrowing of the gap between the vertebrae. The principle of surgical treatment is to remove a defective disc. The recovery period after surgery is about six months. Rehabilitation includes exercise therapy, physiotherapy, and vitamin intake.
Prevention of spinal osteochondrosis consists of combating risk factors - maintaining an active lifestyle, playing sports, proper nutrition, using special corsets and belts when loading the back, sleeping on mattresses and orthopedic pillows, avoiding hypothermia and injury.



































